In a global first, England’s National Health Service is set to roll out a gonorrhoea vaccine, aiming to tackle the escalating rates of this sexually transmitted infection. The innovative program repurposes an existing vaccine to offer protection against a disease that’s becoming increasingly resistant to conventional treatments. This initiative marks a significant step in public health, targeting those most vulnerable to infection and seeking to curb the spread of this concerning illness.
The vaccine being deployed isn’t specifically designed for gonorrhoea. Instead, it’s the meningitis B vaccine (MenB), already part of the routine immunization schedule for babies. Scientists discovered that due to the similarities between the bacteria that cause meningitis B and gonorrhoea, the MenB vaccine offers cross-protection. Studies have indicated that the MenB jab can reduce gonorrhoea cases by approximately a third. While not a silver bullet, health officials see this as a crucial tool in their fight against rising infection rates.
Professor Andrew Pollard, chair of the Joint Committee on Vaccination and Immunisation (JCVI), has emphasized the value of this approach, stating that it is “worth having” and could have “a huge impact” overall.
The initial rollout of the gonorrhoea vaccine will prioritize gay and bisexual men, particularly those with a history of multiple sexual partners or previous STIs. This group is considered at higher risk of contracting the infection. The vaccinations are scheduled to commence in August and will be administered through sexual health services. Public Health Scotland is also formulating its own program to target high-risk individuals within its jurisdiction. Clinicians will retain the discretion to offer the vaccine to other individuals deemed to be at equally high risk when they present at sexual health services.
The urgency of this vaccination program is underscored by the alarming rise in gonorrhoea cases. In 2023, England recorded over 85,000 cases, the highest figure since 1918. Compounding the problem is the increasing antibiotic resistance exhibited by gonorrhoea, making it more difficult to treat effectively. Dr. Amanda Doyle from NHS England highlights the critical importance of the vaccine “in protecting individuals, helping to prevent the spread of infection, and reduce the rising rates of antibiotic-resistant strains of the bacteria.” With concerns growing that gonorrhoea could eventually become untreatable due to antibiotic resistance, prevention is paramount.
Max, a sexual health campaigner, voiced his strong support for the initiative, stating he would “100%” take the vaccine and believes “It’s going to take the pressure off the clinics, it’s just a big win all round.”
The gonorrhoea vaccination program also carries significant economic implications. The vaccine costs approximately £8 per dose, a cost deemed a valuable investment when targeted towards high-risk groups like gay and bisexual men. Projections from Imperial College London suggest that the vaccine could prevent 100,000 cases and save the NHS nearly £8 million over the next decade, assuming widespread adoption. In addition to the gonorrhoea vaccine, individuals will also be offered vaccinations for mpox, HPV, and hepatitis at the same time, maximizing the impact of each visit.
Katie Clark, head of policy and advocacy at the Terrance Higgins Trust, praised the decision as a “huge win.”
Gonorrhoea doesn’t always manifest with obvious symptoms, but when they do appear, they can include pain, unusual discharge, inflammation of the genitals, and, in severe cases, infertility. Early detection and treatment are essential to prevent serious complications.
One consideration is that the vaccine is only 30-40% effective. Therefore, practicing safe sexual practices remains crucial. It is currently unknown how long the protection from the vaccine lasts or how often booster shots may be required.
The introduction of the world’s first gonorrhoea vaccination program by the NHS is a vital step in addressing rising infection rates and the growing threat of antibiotic resistance. While not a panacea, the vaccine represents a crucial preventive measure, particularly for those at higher risk. Continued dialogue with sexual health professionals about ongoing prevention and treatment options remains essential. As Professor Matt Phillips noted, this is “excellent news and a landmark moment for sexual health in England”.
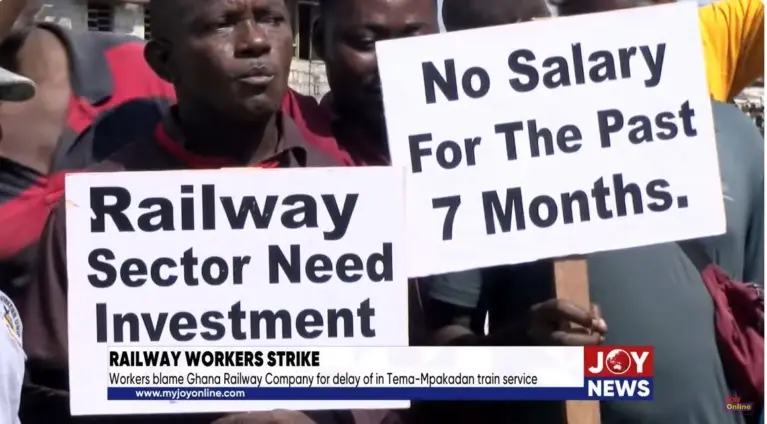
Image Source: MYJOYONLINE